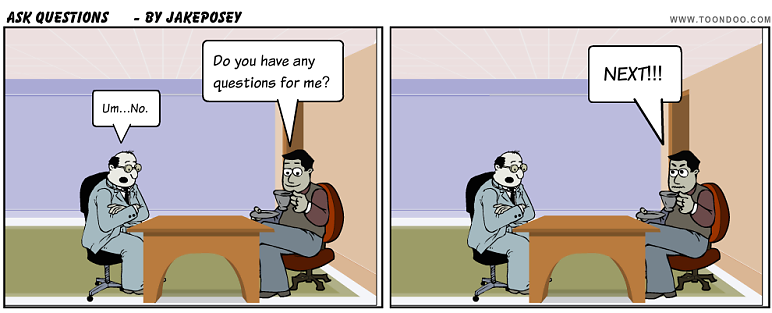
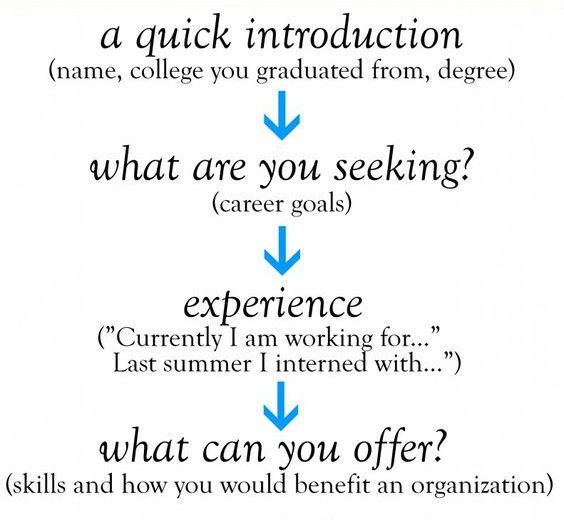
In the last 2 blog posts, we looked at questions that I very much encourage you, the residency applicant, to ask the interviewer. These questions pertain to clinical experience during residency and teaching/learning and research opportunities. Here is the third installment to this post where we add more questions to your bag of questions that you can confidently ask the interviewer and show your interest and commitment to the program where you are interviewing.
"How is my performance evaluated during residency?" "Do I get face-to-face evaluations or written feedback?" "Besides the teaching attendings, are there others such as chief residents or nurses who may be evaluating me?" "Do I have scheduled meetings throughout the year with the program director for feedback?" During residency training, your performance as a physician in training and as a person are being closely monitored at work at all times by your colleagues, medical students, teaching attendings, subspecialty consultants, non-teaching attendings, nurses and hospital staff. Your evaluations during residency are critical in shaping you to be a wonderful physician. If that doesn't motivate you enough, you need to maintain an impeccable profile because residency evaluations are critical in obtaining a fellowship or a clinical practice position in an academic or private setting. Residency evaluations may be available to you in a written form [using platforms such as New innovations] either because of lack of time or interest to have a face-to-face conversation. Make sure you have ample opportunities during residency to receive constructive feedback and do your very best to act on these evaluations.
"What was the boards passing rate for the last class that just graduated?" "Are you satisfied with the boards passing rate for the recent graduates?" "Does the program have separate board review sessions or is it incorporated into the other teaching conferences?" "What resources or board prep materials are provided by the program?" After you complete your residency, you become eligible to take the boards [also called the 'initial certification exam'] administered by ABIM [for internal medicine] and other similar boards to become a "board certified physician". If there is one objective metric that very quickly tells you (and a layman) how effective is the teaching environment and culture in a residency program, it is the Boards pass rate. Every program cherishes to have a 100% boards pass rate. While some may argue that the individual performance on the boards is a reflection of the graduated resident and his or her test taking skills, if a program has a lower than median boards pass rate for that specialty, it needs to implement changes in the teaching curriculum to improve the performance. Here is a link of publicly available board pass rate in internal medicine and you will find a rare program that had a 64% board pass rate, a very concerning program metric. In my opinion, >90% board pass rate is very good.
"Could you let me know about the previous graduates and what career paths - fellowship, research or private practice have they pursued after residency?" This is again a good question to ensure that your career path aligns well with the general trend in the program. For example, if you wish to be a private practitioner in a community practice, then it's not very necessary to work at a large academic medical center that is focused on research grants and publications. To meet your goal in this scenario, you want to be in a community hospital where you will be exposed to different styles of clinical practice. Similarly, if your goal is fellowship or an academic career, then matching at a program that offers no fellowship or limited research opportunities could make you miserable. A lot of programs do provide information on recent graduates on their website or may highlight this information before the interview. However if this has not been discussed, make sure you ask either the program director or any other interviewer. As in my prior post, use all available resources such as the program website, YouTube, Twitter, Facebook to learn as much as you can about the program before you interview.
"Could you let me know how the program helps me match into a fellowship or a clinical practice position after residency?" In the current times with information overload and a lot of noise, it is possible that your stellar application may be ignored by a potential employer. To avoid this, you need to engage the networking skills of your program director another teaching attendings to help you land the position that you desire. Asking this question gives you an idea of how committed and invested is the program in ensuring your success. Are they willing to pick up the phone and market your resume and reach out to their contacts? Or are you going to be on your own? Ask any graduating resident and everyone agrees that this support from the program and the program director works wonders.
"How does the program foster well-being among its residents?" " Am I assigned a mentor during my entire time in residency? Is the mentor in the same or a different specialty?" Residency training can be tiring and arduous. The long work hours, nature of clinical responsibilities, electronic medical record use are alleged to be some of the drivers of burnout. Burnout and emotional distress have generated a lot of discussion in the media. Studies indicate that about 50% of residents experience burnout that some consider to be a precursor to depression. It is absolutely imperative that your mental health and emotional well-being during residency training are in the best shape possible. This allows you to be productive during the long working hours of residency. After you ask this question, assess the interviewer's response to this question. Do they deny that burnout even exists? Are they willing to work with you? Is employee and family assistance program [such as a counselor] available around-the-clock? I myself experienced a distressing situation of a patient death and was able to get back to my life and work after reaching out to EFAP at my hospital. There should be absolutely NO stigma in asking for help. Find out how easily approachable are the program director, chief residents and any other teaching attendings. "Does the program have events to promote collegiality between residents such as social events or outdoor events?" You may also add to this question by letting the interviewer know how you choose to maintain emotional well-being. If you family, friends or relatives in the area who can offer you social support, make sure the interviewer is aware of this fact as this is a strong reason to rank you. If meditation, yoga, exercise, music, art or outdoor events such as hiking or skiing helps you build resilience, do let the interviewer know this. In short, be prepared to answer back if the interviewer asks you about your coping mechanisms.
That is it for now. I hope that these three posts provide you with a variety of questions and the rationale behind asking the interviewer. You don't need to ask each and every question but would be great if you could ask an appropriate question in the right circumstance. For example, if the interviewer is talking about the collegiality among residents and faculty, a question on resident well-being would be most appropriate and so forth. All the best!
The top 10 popular questions will be featured on my next blog posts at https://ed4medllc.blogspot.com/ and the winners will receive a coupon each for a FREE practice interview at Ed4medus.com ! Put those thinking caps on and hurry up!
Photo credit for images in this blog post: https://www.evaluationforms.org/wp-content/uploads/Performance-Evaluation-Form-Feedback.jpg
https://static1.squarespace.com/static/5c468830b105986dd083f052/5c4693bbf950b7a96faf71bf/5d2e06f9cf8a34000150c890/1563369535299/ra-graphic.png?format=2500w
https://ldaamerica.org/wp-content/uploads/2015/05/1370738959078.jpg
https://content.thriveglobal.com/wp-content/uploads/2018/11/GettyImages-175268984.jpg
"How is my performance evaluated during residency?" "Do I get face-to-face evaluations or written feedback?" "Besides the teaching attendings, are there others such as chief residents or nurses who may be evaluating me?" "Do I have scheduled meetings throughout the year with the program director for feedback?" During residency training, your performance as a physician in training and as a person are being closely monitored at work at all times by your colleagues, medical students, teaching attendings, subspecialty consultants, non-teaching attendings, nurses and hospital staff. Your evaluations during residency are critical in shaping you to be a wonderful physician. If that doesn't motivate you enough, you need to maintain an impeccable profile because residency evaluations are critical in obtaining a fellowship or a clinical practice position in an academic or private setting. Residency evaluations may be available to you in a written form [using platforms such as New innovations] either because of lack of time or interest to have a face-to-face conversation. Make sure you have ample opportunities during residency to receive constructive feedback and do your very best to act on these evaluations.
"What was the boards passing rate for the last class that just graduated?" "Are you satisfied with the boards passing rate for the recent graduates?" "Does the program have separate board review sessions or is it incorporated into the other teaching conferences?" "What resources or board prep materials are provided by the program?" After you complete your residency, you become eligible to take the boards [also called the 'initial certification exam'] administered by ABIM [for internal medicine] and other similar boards to become a "board certified physician". If there is one objective metric that very quickly tells you (and a layman) how effective is the teaching environment and culture in a residency program, it is the Boards pass rate. Every program cherishes to have a 100% boards pass rate. While some may argue that the individual performance on the boards is a reflection of the graduated resident and his or her test taking skills, if a program has a lower than median boards pass rate for that specialty, it needs to implement changes in the teaching curriculum to improve the performance. Here is a link of publicly available board pass rate in internal medicine and you will find a rare program that had a 64% board pass rate, a very concerning program metric. In my opinion, >90% board pass rate is very good.
"Could you let me know about the previous graduates and what career paths - fellowship, research or private practice have they pursued after residency?" This is again a good question to ensure that your career path aligns well with the general trend in the program. For example, if you wish to be a private practitioner in a community practice, then it's not very necessary to work at a large academic medical center that is focused on research grants and publications. To meet your goal in this scenario, you want to be in a community hospital where you will be exposed to different styles of clinical practice. Similarly, if your goal is fellowship or an academic career, then matching at a program that offers no fellowship or limited research opportunities could make you miserable. A lot of programs do provide information on recent graduates on their website or may highlight this information before the interview. However if this has not been discussed, make sure you ask either the program director or any other interviewer. As in my prior post, use all available resources such as the program website, YouTube, Twitter, Facebook to learn as much as you can about the program before you interview.
"Could you let me know how the program helps me match into a fellowship or a clinical practice position after residency?" In the current times with information overload and a lot of noise, it is possible that your stellar application may be ignored by a potential employer. To avoid this, you need to engage the networking skills of your program director another teaching attendings to help you land the position that you desire. Asking this question gives you an idea of how committed and invested is the program in ensuring your success. Are they willing to pick up the phone and market your resume and reach out to their contacts? Or are you going to be on your own? Ask any graduating resident and everyone agrees that this support from the program and the program director works wonders.
"How does the program foster well-being among its residents?" " Am I assigned a mentor during my entire time in residency? Is the mentor in the same or a different specialty?" Residency training can be tiring and arduous. The long work hours, nature of clinical responsibilities, electronic medical record use are alleged to be some of the drivers of burnout. Burnout and emotional distress have generated a lot of discussion in the media. Studies indicate that about 50% of residents experience burnout that some consider to be a precursor to depression. It is absolutely imperative that your mental health and emotional well-being during residency training are in the best shape possible. This allows you to be productive during the long working hours of residency. After you ask this question, assess the interviewer's response to this question. Do they deny that burnout even exists? Are they willing to work with you? Is employee and family assistance program [such as a counselor] available around-the-clock? I myself experienced a distressing situation of a patient death and was able to get back to my life and work after reaching out to EFAP at my hospital. There should be absolutely NO stigma in asking for help. Find out how easily approachable are the program director, chief residents and any other teaching attendings. "Does the program have events to promote collegiality between residents such as social events or outdoor events?" You may also add to this question by letting the interviewer know how you choose to maintain emotional well-being. If you family, friends or relatives in the area who can offer you social support, make sure the interviewer is aware of this fact as this is a strong reason to rank you. If meditation, yoga, exercise, music, art or outdoor events such as hiking or skiing helps you build resilience, do let the interviewer know this. In short, be prepared to answer back if the interviewer asks you about your coping mechanisms.
That is it for now. I hope that these three posts provide you with a variety of questions and the rationale behind asking the interviewer. You don't need to ask each and every question but would be great if you could ask an appropriate question in the right circumstance. For example, if the interviewer is talking about the collegiality among residents and faculty, a question on resident well-being would be most appropriate and so forth. All the best!
Before you go: Here's your golden opportunity to have your voice heard! Write down your ONE question regarding your US residency program application, personal statement, interviews or anything that has been bothering you and keeping you up at night. You can reply at the end of this post or message at my Facebook page or email me at varun@ed4medus.com
The top 10 popular questions will be featured on my next blog posts at https://ed4medllc.blogspot.com/ and the winners will receive a coupon each for a FREE practice interview at Ed4medus.com ! Put those thinking caps on and hurry up!
Photo credit for images in this blog post: https://www.evaluationforms.org/wp-content/uploads/Performance-Evaluation-Form-Feedback.jpg
https://static1.squarespace.com/static/5c468830b105986dd083f052/5c4693bbf950b7a96faf71bf/5d2e06f9cf8a34000150c890/1563369535299/ra-graphic.png?format=2500w
https://ldaamerica.org/wp-content/uploads/2015/05/1370738959078.jpg
https://content.thriveglobal.com/wp-content/uploads/2018/11/GettyImages-175268984.jpg